Get a plan made for your unique body and goals
Celiac Disease: Symptoms, Causes, and the Latest Treatment Insights

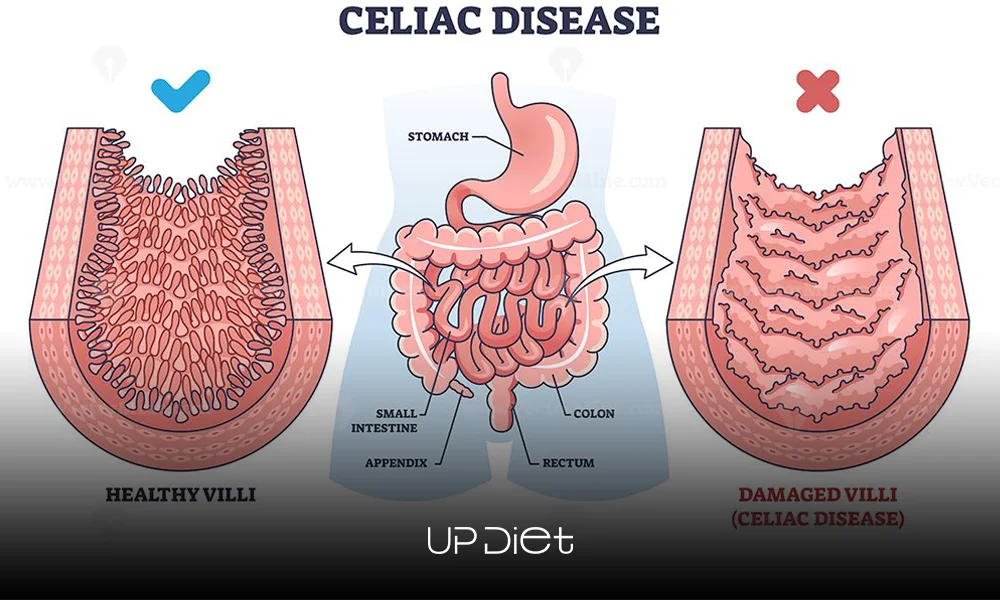
Celiac disease is an autoimmune reaction to gluten. When ingested, the immune system mistakenly attacks the small intestinal villi, impairs their nutrient absorption, and causes further complications.
Today, we’re going to take a closer look at this condition and how it differs from common gluten allergies. We’ll also cover its diagnostic and treatment methods, safe foods for people with celiac disease, and the long-term risks if left untreated.
What Causes Celiac Disease?
The primary genetic factors associated with celiac disease are the HLA-DQ2 and HLA-DQ8 genes, which are present in nearly 95% of individuals with this condition.
It can also be activated in genetically susceptible people through environmental triggers such as viral infections, stress, and changes in diet or gut microbiota.
Symptoms of Celiac Disease
Intestinal villi are responsible for absorbing nutrients, fats, proteins, carbohydrates, vitamins, and minerals. Their damage leads to malabsorption and a variety of common symptoms, including:
- Bloating and gas
- Diarrhea or constipation
- Nausea and vomiting
- Abdominal pain
- Fatigue
- Anemia
- Skin rashes (DH or dermatitis herpetiformis)
- Headaches
- Weight loss
- Neurological symptoms like muscle weakness or paresthesia
- Reproductive issues such as infertility or miscarriage
Celiac Disease vs. Gluten Sensitivity: What’s the Difference?
Celiac disease and non-celiac gluten sensitivity (NCGS) are both associated with gluten consumption. Still, their mechanisms and impact on health are entirely different.
Celiac disease is an autoimmune disorder where gluten triggers an immune response that causes inflammation and damage to the small intestine’s villi. This impairs the body’s ability to absorb nutrients, leading to long-term complications such as malnutrition, osteoporosis, and even cancer.
Non-celiac gluten sensitivity doesn’t involve an autoimmune response. People with NCGS experience symptoms similar to celiac disease (bloating, abdominal pain, fatigue, etc.), but without the damage to their intestine. That’s why NCGS doesn’t have increased long-term risks, although it can be pretty uncomfortable.

How Celiac Disease Is Diagnosed
A recent NIH study advises clinicians to identify gastrointestinal and extraintestinal symptoms, along with physical examination findings from:
- Blood tests: Initial screening involves measuring antibodies like tTG-IgA (tissue transglutaminase IgA) and EMA (endomysial antibodies). These tests are highly sensitive and help identify individuals who may have celiac disease.
- Total IgA levels: This test checks for immunoglobulin A deficiency, as low levels can affect the accuracy of the tTG-IgA test.
- Endoscopy and biopsy: The gold standard for diagnosis is an upper gastrointestinal endoscopy with biopsy, where a tissue sample from the first part of the small intestine (duodenum) is examined for villous atrophy or damage to the villi.
These tests are recommended for anyone with at least one of the following symptoms: persistent, unexplained gastrointestinal issues, faltering growth, or prolonged fatigue.
Celiac Disease Foods: What to Eat and Avoid
Important Note! Always read product labels on celiac disease foods to ensure there’s no hidden gluten. Also, be careful about cross-contamination in shared kitchens through utensils, cutting boards, cooking surfaces, or even airborne flour.

Latest Treatment Insights
A study on PubMed titled “New Insights in Celiac Disease” states that the only effective treatment is a lifelong, strict gluten-free diet (GFD), which helps heal the intestinal lining and manage symptoms.
Emerging research also explores additional treatments, such as enzyme therapy (to break down gluten effectively and reduce its effects on the digestive tract), microbiome modulation (balancing gut microbiota to reduce immune responses), and immune tolerance (to induce tolerance to gluten, not yet available for general use).
Long-Term Risks if Untreated
Undiagnosed, uncontrolled celiac disease can lead to serious health complications and severely impact quality of life and longevity, including:
- Osteoporosis due to poor calcium absorption
- Malnutrition, especially deficiencies in vitamins and minerals
- Anemia from iron deficiency
- Delayed growth in children
- Increased risk of other autoimmune disorders (like Type 1 diabetes, thyroid disease)
- Intestinal lymphoma and other cancers
Final Thoughts
Managing celiac disease requires a lifetime adherence to a gluten-free diet. This is the most effective way to manage symptoms while preventing health issues.
Personalized nutrition can make this commitment much easier. Tools like UP-Diet create customized meal plans for celiac disease, so you can stay consistent in the long run and feel your best every day.
- In this post:
- What Causes Celiac Disease?
- Symptoms of Celiac Disease
- Celiac Disease vs. Gluten Sensitivity: What’s the Difference?
- How Celiac Disease Is Diagnosed
- Celiac Disease Foods: What to Eat and Avoid
- Latest Treatment Insights
- Long-Term Risks if Untreated
- Final Thoughts



